Over the past three years, I have written extensively on the criticality of being informed and prepared and at no time has the need for this been more apparent than now. Many have contacted me asking, “What do I do now?” “Is it too late to be prepared?” The answer is it is never to late to start to put plans in place. There is an immediate need to plan for the ongoing impact and disruption in our lives and of those entrusted to our care.
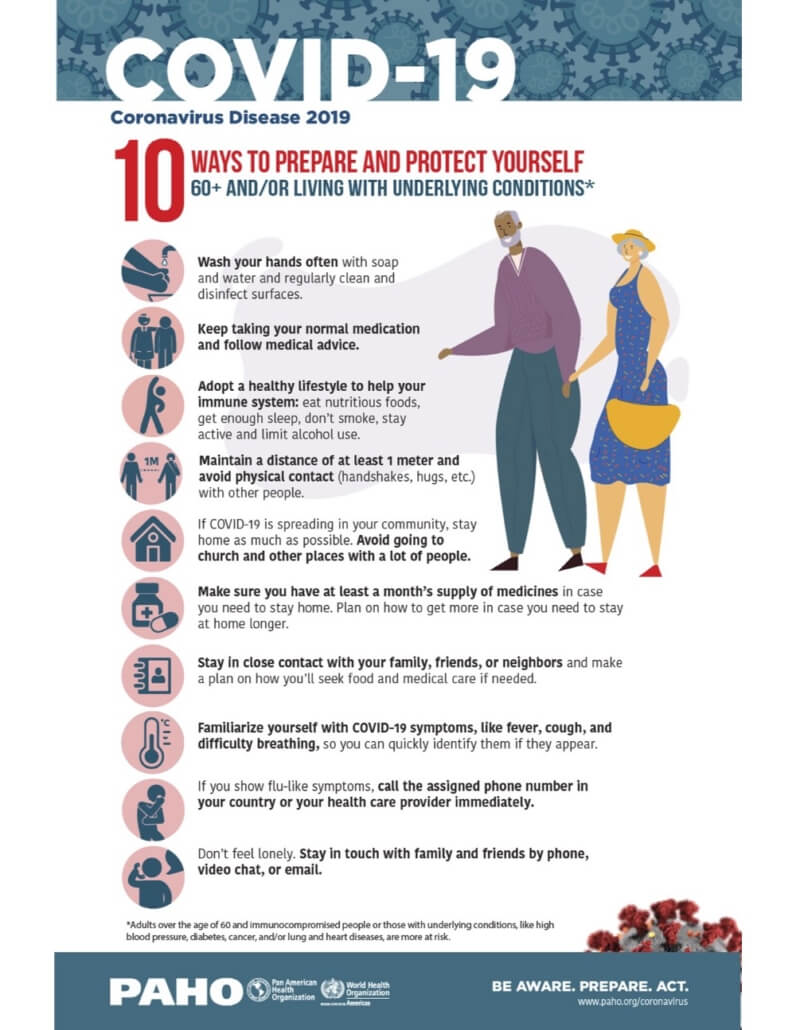
For Seniors this is a “Must do” versus a “Nice to do.” The World Health Organization has extensively written on the roles and risks for the aging population in times of emergency. Loss of independence or even a loss of life occurred way too often in many of the crises in the last decade. With the evidence from Italy and China, the impact of coronavirus on the elderly population will be even more significant.
Here are the 6 critical Objectives for Orchestrating Care in a Crisis
1. Define basic needs
2. Be connected to the world at large
3. Maintain your lifelines to others / engage in Life
4. Create a safe and secure space
5. Document what is going on
6. Create a disaster plan and know when to implement
1. Define basic needs
Know your basic needs and your primary needs and devise a back up strategy for both. We recommend a focus on the following 13 areas.
Can you:
1. Get bills paid
2. Get groceries / household supplies
3. Have meals prepared
4. Get help if needed
5. Get laundry done
6. Take garbage out
7. Maintain clean food preparation space
8. Get house cleaned
9. Get transportation to necessary places
10. Use the phone
11. Have general mobility in the living environment and in places critical to visit
12. Get Activities of Daily Living (ADLs) met (e.g. bathing, grooming, toileting, ambulation, etc)
13. Manage your medical condition (get meds, dose meds, take as prescribed, manage vitals within defined parameters and escalate if needed.)
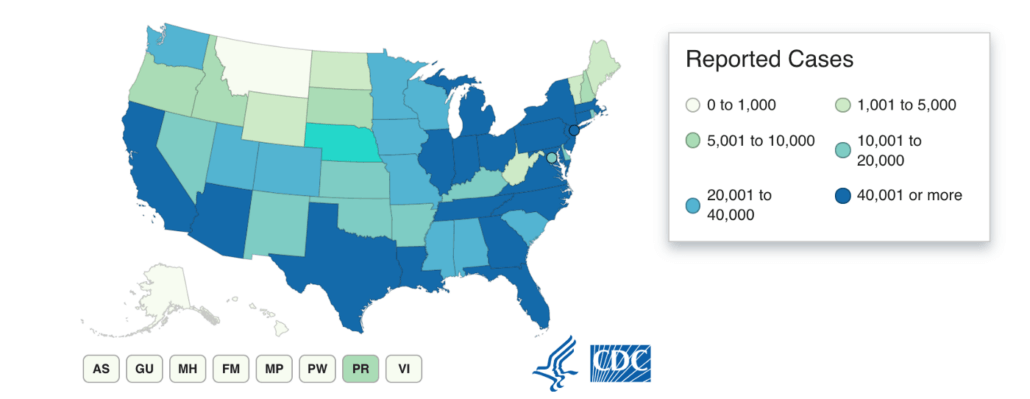
2. Be connected to the world at large
The importance of a plan B is paramount in times of disruption. For most, plan B and often Plan C, also known as “Uh oh, now what,” relies on being able to quickly navigate many options on a moment’s notice. Think about our reliance today on the internet to get things done. Whether a home-based connection or via a mobile phone or tablet, connectivity is a necessity in today’s world. That said many, especially Seniors, do not have sufficient connection.
Over the past two years, my home care agency and our franchisor have sought various technology-based care enhancements for our clients. Our goal was simple; can we provide a greater level of care or oversight at a lower cost through the use of technology to separate care? The results were quite surprising. While nearly everyone had smart (or smarter) phones and could text, facetime or the equivalent, a surprising number (over half) did not have active internet service in their home. The challenges of our Covid19 day-to-day existence have clearly demonstrated internet access is a necessity.
Review the 13 basic needs above, how could you ensure these were adequately met without internet access? It would be possible, but it would be difficult — particularly in times of mass need and disruption as we face today.
3. Maintain your lifelines / Engage in Life
Per AARP, “Social distancing shouldn’t mean shutting out the world. We all need human connection, particularly in a crisis and especially with those who understand and care about us. Research has shown just how emotionally and physically harmful social isolation can be. Fortunately, we live in a miraculous age when we have a myriad of technological means — including telephone, email, texting, video chat and social media — to keep our friends and family members present in our lives. That may be the best available solace for all of us until this crisis passes.”
Three types of needed lifeline connections
1. A responsible person who can escalate on your behalf: Set a specific person who you speak to each day at a specific time. Have a daily check in and give basic information so they can intervene if necessary or, if you fail to check in, know to call 911 on your behalf. The three areas we recommend are:
a. Your well being — BE HONEST about your ability to meet your 13 basic needs.
b. Your state as it relates to other needs that you are having trouble meeting
c. Changes they should be aware of (i.e., medication routines, appointments, etc.)
2. Connection to professionals you may need to access. Increasingly our medical professionals are communicating by dedicated websites or applications on our phones that allow us to communicate with them and for them to respond. The general ability to get a doctor or their staff, even in an emergency, is difficult and in a peak demand due to a crisis — likely impossible. These applications and sites ensure your doctor will get your message and can respond.
3. General connection to others: Stay connected to your friends and loved ones. Set call times up — make a plan. Set up a video chat or even a group one. These things are quite easy if someone shows you how. Email or social media is a great way to stay in touch and find out how things are going. AARP wrote: “Share moments of mutual enjoyment and meaning”. Even in coronavirus confinement, upbeat instances still go some ways toward offsetting frictions both small and large. Put on the old movies or music that you always enjoyed together. Bring out the photo albums to remind you of wonderful vacations and family gatherings of the past. Make and savor the recipe that was always a family favorite. Sit together on the living room couch in silence holding hands.
(Note the importance of a reliable internet connection in maintaining lifelines especially in times of social distancing or sheltering in place. )
4. Create a safe and secure space that allows separation
I have written about the 144 potential safety risks in the home. Now is the time to minimize these risks. Not all of us or our environment have the full list but here is a way to think about it:
1. The Bathroom: Remove un-necessary clutter. Make sure non-slip tape is where it needs to be and that assistive devices are in place — grab bars. Make sure the things your need are in easy reach.
2. The Bedroom: Remove un-necessary clutter. Pick up loose items on the floor. Please consider removing things that could pose a fall risk. For example, loose throw rug or things that are hard to see in the dark.
3. The kitchen: Remove un-necessary clutter. Make sure basic kitchen / food prep needs are in reach so you can avoid the use of a stool to get things. Have food storage needs in place (Ziploc bags, resealable containers). It is recommended that staple canned goods are available — not hoarding quantities — but to have if needed.
4. Separation: If the size of your world has shrunk to the confines of your home, then it is crucial to figure out ways to carve out time and space that’s still yours. Taking 20 minutes to go to a separate room from the person you’re caring for or living with helps you clear your mind and recover a little. Even if you must be in the same room all the time, there may be ways to focus on your own needs. Read a book or listen to calming music with headphones as an example. There are many small ways to be present and available but also separate and self-contained.
5. Document what is going on
Remember when we were kids. Many kept a diary or a log of the most significant and or insignificant things going on. Keep a diary but keep it focused. Document how your day is, how you feel, who you spoke to. Capture what you are concerned about and who you should discuss it with. (Remember your daily calls — don’t leave the important stuff out.). During times of chaos and stress, it is always best to have detailed notes to refer to rather than rely solely on memory. Document all these things so you have a good record.
6. Create a disaster plan
No matter where you live, have a disaster plan ready for you and those you care for.
Your plan should include a written list of current needs, routines and impairments. It should include all identifying information (date of birth, Social Security number and a current photo) as well as allergies, medications and diagnoses. Prepare a biography of your loved one that will better inform providers of their personality, interests and background. This is especially important for medical conditions where you or a loved one relies on others to be their “voice.”
Consider where you could relocate in the event of need. Most importantly confirm its availability to you and how they can communicate if availability changes. Ensure they can meet your needs not just your shelter.
Some final thoughts
These are trying times. We are all managing stress, anxiety, uncertainty. When we have enforced round-the-clock together time it is easy for things to escalate. There are everyday frictions both small and large that all have the potential to escalate — resist the urge. I find myself saying I’m sorry a lot — it is sincere, even when I am not sure what I have done. I am sorry that I did something that caused stress on the other person. Don’t beat yourself up, don’t put down others.
Be kind to yourself, be kind to others. You never know what is going on in someone else’s life, so let’s all remember not to judge and most importantly to be kind. Viruses are contagious but so is bad attitude and aggression. But more importantly, so is kindness, empathy and support. Pay it forward, because you just don’t know how the return can positively impact you or your loved one.
Let’s all leave good footprints where we tread!